Top Causes of Finger Pain — Symptoms, Triggers & Treatment Tips
By Dr. M. Zannakis | The CarpalRx
Finger pain can arise from injuries, arthritis, nerve compression, or infections. Common causes include sprains, fractures, tendonitis, carpal tunnel syndrome, trigger finger, and joint inflammation. Understanding symptoms like swelling, stiffness, or tingling can help you pinpoint the cause and seek proper care.
Table of Contents
- Characteristics of finger pain
- Pain with swelling
- Pain upon movement
- Pain at the injury site
- Pain accompanied by a lump
- Top 12 Causes of Finger Pain
1) Finger injury
2) Arthritis
3) Carpal Tunnel Syndrome
4) Peripheral Neuropathy
5) De Quervain's Tenosynovitis
6) Gout
7) Dactylitis
8) Scleroderma
9) Trigger Finger
10) Ganglion Cyst
11) Raynaud's Disease
12) Lupus
Overview
There can be many causes of finger pain ranging from trauma to a host of ailments. To determine which one is causing yours it’s important to describe the
characteristics of that pain. For instance:
- Is the pain constant or intermittent?
- Does it feel like sharp stabs or a continuous dull ache?
- Does it burn or itch?
- Do you see any physical changes on your skin?
These characteristics can help pinpoint the cause of your finger pain. Usually, the reason for the pain has a simple or obvious explanation, like physical injury or trauma. Other times, pain can be a symptom of a more complicated disorder like carpal tunnel syndrome.
The top 12 causes of finger pain are listed below
-- in order from most common to least common. You’ll also find more information about each cause and the best way to help relieve that condition.
WARNING!
Some cases of hand or finger pain may need immediate attention. Call your doctor if you feel any of the following:
- You cannot move your finger or grasp objects.
- Extremely severe hand or finger pain occurs suddenly, makes you feel dizzy, faint or sick.
- You have lost feeling in your finger or hand after an injury or felt a pop, snap or grinding after the injury.
- Your finger has changed color or has noticeably changed shape.
Characteristics of finger pain
Hand or finger pain can give you different feelings. They range from achy and dull to sharp and stabbing. Sometimes they feel like a cramp or even burning.
Also, the pain may be intermittent or constant. Sometimes it may start suddenly, then disappear. Any of these pain qualities can apply the types of pain listed directly below.
Pain with swelling
Having finger pain with swelling can be the sign of a broken bone (see cause 1. Finger Injury,
below). That's especially true immediately after an injury. Usually the skin changes from its normal color to blue or purple. A broken bone is very painful and unmistakable. Sometimes the broken bone is visible through the skin (called a compound or open fracture).
Pain upon movement
Some disorders cause throbbing pain when you move a finger. The most common conditions are advanced carpal tunnel syndrome, tendonitis or tenosynovitis, and arthritis (these are discussed below). Carpal tunnel syndrome also makes fine movements difficult, and may cause
shooting electric shocks, or sharp stabbing pain.
A finger dislocation is when bones misalign with their joints. In some instances the misalignment is clearly visible because the
finger is crooked.
Pain at the injury site
A burn or cut on your hand or finger can cause pain at the injury site. The severity of the burn or cut may cause pain to spread from the injury.
Pain accompanied by a lump
A lump (boil or nodule) on your hand or finger can cause pain. The lump can be fluid-filled, hard, moveable or tender to the touch. Treatment depends what's causing the lump and how severe your symptoms are. Most times, the lump resolves on its own.
Top 12 Causes of Finger Pain
1. Finger Injury
By far, injury or trauma to the fingers or hand is the leading cause of finger pain. Over a million American workers
report hand or finger injury each year. Of course, the number of people who do not report such injury on the job is probably many times greater than that number.
The types of traumas to the hand and fingers range widely. They can be simple cuts, scrapes, punctures or mild burns. But they can also be serious injuries like deep lacerations, severe abrasions, deep burns, finger crushes, and fractured bones.
Treating Finger Injury
Most hand or finger pain due to injury can be treated easily. First, stop any bleeding with firm pressure and then apply a bandage. If the damage is more extensive, apply ice to reduce inflammation. Direct compression can help stop bleeding. Elevating your hand can also help control bleeding.
2. Arthritis
Osteoarthritis (OA) is also called
degenerative joint disease. It causes pain, stiffness, and swelling at the joints due to cartilage breakdown. OA is most common in the smaller joints of the fingers. It usually develops with age which is why it's referred to a “wear and tear” disorder. However, it may also develop faster following an injury.
A related condition,
rheumatoid arthritis (RA) is an inflammatory autoimmune disorder. It’s when your body attacks its own healthy joints. It is most often seen in the wrists, fingers, spine, and knees. RA usually worsens during periods of
“flare-ups”. These cause increased pain, swelling, redness, and stiffness in the joints.
Treating Arthritis
While there is no cure for OA, topical pain medicines and oral pain relievers help. In addition, hot and cold packs, exercise, weight loss, and healthy eating have tremendous effects in reducing symptoms. RA can be treated using immunosuppressive therapies, which include methotrexate and biologics.
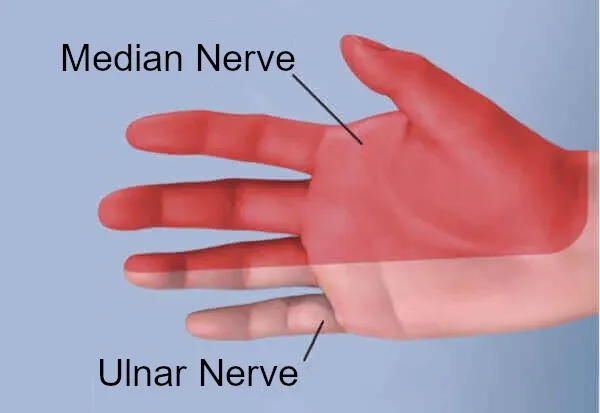
3. Carpal Tunnel Syndrome
Carpal tunnel syndrome is one of the
major causes of finger pain. It is a type of
peripheral neuropathy (see next cause below) caused by compression of the
median nerve inside the wrist joint. The compression occurs because
flexor tendons become irritated and begin to swell. Thus, carpal tunnel syndrome is a result of
inflamed flexor tendons.
The symptoms of carpal tunnel syndrome vary from person to person. The symptoms are always on the palm side of the hand and/or the fingers (never the pinky finger). These symptoms include
pain,
numbness, tingling,
weakness, clumsiness,
burning,
shooting electric shocks, and itching.
Nobody is really certain why carpal tunnel syndrome occurs in some people but not in others. However, the major risk factors for acquiring carpal tunnel syndrome are
occupations requiring
strenuous or harmful hand activity, rapid and repetitive finger activity,
pregnancy, or having prolonged (and/or poor)
sitting posture.
Treating Carpal Tunnel Syndrome
Finger pain due to carpal tunnel? Stop the pain - try the CarpalRx!
4. Peripheral Neuropathy
Peripheral neuropathy occurs when nerves of your arms, hands, fingers, legs, feet, and toes are damaged. With peripheral neuropathy of the hand, it results in
symptoms like hand or finger pain, numbness, tingling (pins-and-needles), burning, and reduced sensation.
Damage to nerves can result from injury,
diabetes,
vitamin deficiency,
peripheral vascular disease, infection, and
Guillain-Barré syndrome. Peripheral neuropathy may also be a side effect of certain
chemotherapies.
Treating Peripheral Neuropathy
Doctors treat peripheral neuropathy according to the cause of the disorder. For instance, vitamin deficiency can be treated with
oral supplements.
Diabetic neuropathy can be treated by careful monitoring blood glucose. Early diagnosis is crucial. Since nerves are not very sensitive to change, any treatments may only halt the progression, but not reverse the nerve damage. Drugs to control peripheral neuropathy symptoms include
gabapentin (Neurontin),
duloxetine (Cymbalta), and
pregabalin (Lyrica).
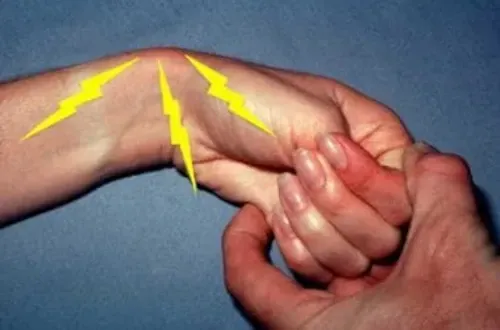
5. De Quervain’s Tenosynovitis
De Quervain's tenosynovitis (also called de Quervain’s syndrome or de Quervain’s disease) is a painful inflammation of the tendons in your lower thumb and wrist. Your thumb tendons pass through a
narrow tunnel in that area. When the tendons swell, they rub against the tunnel wall. This, then produces pain at the base of your thumb – often radiating into your forearm.
The exact cause of de Quervain's tenosynovitis is unknown. But the disorder seems to result from one of the following: a direct hit to the thumb,
gaming, activities requiring
prolonged gripping, rheumatoid arthritis, and
repetitive stress.
You can test for de Quervain's tenosynovitis using the
Finkelstein test. Make a fist with your thumb inside. Then bend your fist in the direction of your little finger. Pain at the indicated area in the photo is positive for this condition.
Treating de Quervain's Tenosynovitis
Reducing tendon inflammation is the key to relieving symptoms of de Quervain’s tenosynovitis. This can be achieved with
drugs such as ibuprofen or naproxen. Your doctor can also give you a corticosteroid injection in to the tendon’s sheath to ease the swelling.
Steroid injections are most effective when symptoms are new (within 6 months). In addition, immobilization of your thumb with a
thumb splint for 4-6 weeks may also help. Finally, daily
gentle massaging and
light thumb exercises can break restrictions on the tendon and help relieve pain.
6. Gout
Gout is a common and painful type of arthritis. It results in swollen, hot, red, and stiff joints. The condition occurs when
uric acid builds up in the body. Uric acid results from eating
foods like liver, anchovies, and dried beans or peas. Gout happens when the uric acid doesn’t normally dissolve in the blood. Instead, it forms sharp, stabbing crystals - like broken glass. When the crystals are located in your joints, it becomes very painful. The same crystals can also produce
kidney stones.
Most times, gout first attacks the big toe. It can also affect the ankles, heels, knees, elbow, wrists, and fingers. As it begins, pain can come and go. But I time, it occurs more often.
Risk factors for having gout include: being male, a family history of gout, diabetes, obesity, excessive alcohol consumption,
congestive heart failure,
kidney disease, and eating
foods rich in purines (like red meat).
Treating Gout
7. Dactylitis
Dactylitis is condition where swelling of your fingers or toes gives them a sausage-like appearance. This condition is associated with an autoimmune inflammatory form of arthritis called
psoriatic arthritis. Dactylitis can cause fingers or toes to be painful, red, and swollen.
Treating Dactylitis
Dactylitis usually will not resolve on its own. Most doctors advise using Nonsteroidal Anti-inflammatory Drugs (NSAIDs) to ease the pain and swelling. Other more powerful drugs the doctor may prescribe are
Meloxicam,
Nabumetone or
Sulindac.
8. Scleroderma
Scleroderma is a disorder that produces a thickening and hardening of the skin (as well as other organs). It happens because your body
over-produces collagen. The most obvious sign of scleroderma it the production of toughened and shiny skin. It also can cause pain, stiffness, and swelling in the finger joints.
Treating Scleroderma
There is no way to prevent the overproduction of collagen which causes scleroderma. But various drug treatments can help control the symptoms and even prevent complications. Some drugs are simple pain relievers. But since scleroderma can affect various parts of the body, the choice of other drugs will depend on your symptoms. For instance, drugs which dilate blood vessels (i.e.,
hypertension medicines) can help treat
Raynaud's phenomenon ("white finger"). Other drugs help
suppress the immune system, which in turn help reduce progression of some scleroderma symptoms like skin thickening. Yet other drugs can help reduce
digestive symptoms like heartburn.
Infection control is also an important aspect of scleroderma treatment. Protection from the cold, as well as skin cleaning can help prevent fingertip infection from ulcers due to Raynaud's disease.
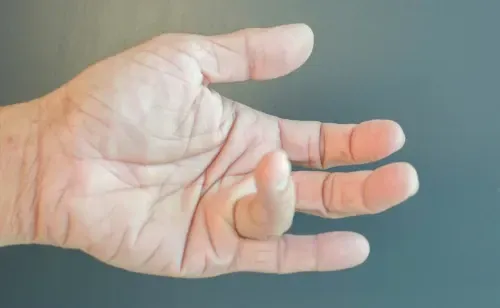
9. Trigger Finger
Trigger finger (or
stenosing tenosynovitis) is when the
sheath surrounding a tendon inflames. This causes the inner tendon itself to “catch” when you try moving the finger.
Trigger finger commonly occurs at the base of the finger. The most common symptoms are a catching or popping feeling when you move a finger. As the finger moves, it reaches the trigger point, whereupon it "releases" so you can move it freely again. It might be difficult to bend or fully straighten your finger.
Trigger finger may also be accompanied by pain. The trigger area may be especially painful to the touch. It may also be swollen. Many patients also feel stiffness or
cramps in their finger. Long periods of inactivity can make symptoms worse.
The causes of trigger finger are not well understood. But some conditions like diabetes or rheumatoid arthritis can increase your risk of developing it.
Treating Trigger Finger
The best way to treat trigger finger is to
gently massage the area where you feel the “catch”. Massage for 5 minutes. This should be done several times per day. In addition, regular
finger stretching exercises will relieve stiffness. More serious cases of trigger finger pain may require a
steroid injection. This reduces inflammation and pain. The
most
serious conditions of trigger finger may require
surgery to release the tendon from its sheath.
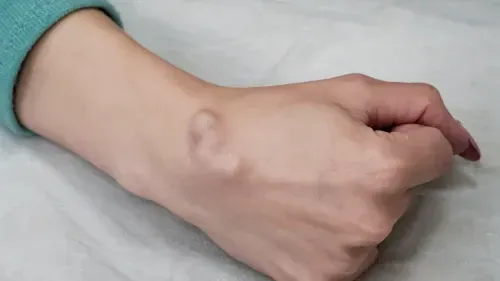
10. Ganglion Cysts
A
ganglion cyst is a fluid-filled bump beneath the skin. It is most often found over a tendon or joint in the hand or wrist. A ganglion cyst forms when there is a small rip in the
sleeve of thin tissue that covers a joint or tendon. The tissue bulges and forms a sac. Fluid from the joint leaks into the sac and causes swelling.
A ganglion cyst usually is more irritating than painful. Symptoms include a visible, smooth lump on the skin. You may also have one of the following: pain or pressure when bending the joint, tingling or numbness, and reduced range of motion.
Treating Ganglion Cysts
Most ganglion cysts resolve without treatment. But some may return after treatment. If the cyst is not painful, a watch-and-wait approach may be best. If the ganglion cyst is causing pain, there are several treatment options. First, a brace can be use to immobilize the cyst. This helps prevent additional irritation when your joint moves.
Aspiration of the cyst maybe helpful. That's when the fluid is drained from the cyst using a fine needle. The cyst may or may not fill with fluid again. If none of these treatments work, then
surgical excision of the ganglion cyst is recommended. But excision does not guarantee the cyst won’t return.
11. Raynaud's Disease
A rare disorder of the blood vessels,
Raynaud's disease usually involves the fingers and toes. Sometimes Raynaud's disease is called "white finger" disorder. The blood vessels in those areas become narrow when you are exposed to cold or feeling
emotionally stressed. When this occurs, blood can't reach the skin’s surface, and the affected area turns white and blue. When blood flow returns, the skin turns red and tingles or throbs. In more severe cases of Raynaud’s disease, loss of circulation can cause sores or even tissue death.
Primary Raynaud's happens by itself, where the cause is not known.
Secondary Raynaud's is caused by injuries, some drugs, or other diseases. Raynaud’s is more common in people living in cold climates. It is also more common in people with a family history of the disorder, women, and people over 30 years old.
Treating Raynaud's Disease
Treatment for Raynaud’s disease will depend on the severity of the condition and whether you have the primary or secondary form. The
treatment goals are prevention of attacks, severity reduction, treating the underlying condition (for secondary Raynaud’s), preventing skin ulcers, and improving quality of life. For many patients, making lifestyle changes are enough to manage the disorder. Such changes include avoiding cold places, avoid touching cold objects, managing stress, and wearing warm clothing. With more severe symptoms, certain drugs may also help.
Calcium-channel blockers can be used to relax small blood vessels. They also can help heal skin ulcers on the fingers and toes.
Alpha-blockers can also be used to constrict blood vessels. Finally,
nitroglycerin skin ointment can be applied topically to help heal skin ulcerations.
12. Lupus
Lupus (or
systemic lupus erythematosus) is a chronic autoimmune disease. It can produce swelling and pain throughout your body. An autoimmune disease means that your body’s immune system is fighting itself, especially healthy tissue.
Lupus causes joint pain, skin sensitivity, and rashes. It also causes problems with internal organs such as the brain, lungs, kidneys, and heart. It’s common for symptoms to come and go, called
flare-ups. Symptoms can be mild or not even noticeable. But they can also be so severe they adversely affect your daily life.
Lupus is
ten times more common in women. There are several types of the disorder. The most common is systemic lupus erythematosus. Others are
cutaneous lupus erythematosus (affecting the skin) causing sun sensitivity, rashes, and hair loss.
Drug-induced lupus is caused by certain medications, and usually resolves when the drug is removed.
Neonatal lupus is rarer, and found in infants at birth.
Treating Lupus
The way lupus is treated depends on
several factors. These include which symptoms (or complications) you have, its severity, your age, the kinds of drugs you are taking, and your overall health and history. The general goal is to bring symptoms into remission. This is a life-long fight, and must be monitored regularly by your doctor. Patients with mild symptoms usually require limited treatment. Most treatments usually focus on drug therapy. They include
topical steroids for skin rashes,
hydroxychloroquine (Plaquenil),
azathioprine (Imuran),
methotrexate (Rheumatrex),
cyclophosphamide (Cytoxan),
mycophenolate mofetil (CellCept),
belimumab (Benlysta), and
rituximab (Rituxan).
Summary
Finger pain can come from many sources — from simple overuse to chronic conditions like
carpal tunnel syndrome,
arthritis, or
nerve compression. The pain might feel sharp, dull, or throbbing and may occur with stiffness, swelling, or tingling. Because your fingers contain delicate joints, tendons, and nerves, even minor irritation can cause significant discomfort. Understanding the underlying cause is essential for proper treatment. In many cases, gentle
myofascial release therapy—like the therapy provided by the
CarpalRx device—can relieve pain by improving circulation and reducing tissue tension around the wrist and fingers.
FAQs
1. What causes finger pain without injury?
Finger pain without an injury often results from conditions such as
carpal tunnel syndrome,
arthritis, or
nerve compression in the wrist or forearm. Repetitive motions and poor wrist posture can also trigger inflammation that radiates into the fingers.
2. Can carpal tunnel syndrome cause finger pain?
Yes. Carpal tunnel syndrome commonly causes pain, tingling, or numbness in the thumb, index, middle, and part of the ring finger. The discomfort originates from pressure on the median nerve inside your wrist.
3. How can I relieve finger pain naturally?
Gentle stretching, regular breaks from repetitive work, and
myofascial release massage using devices like the
CarpalRx can provide quick, non-surgical relief. Applying cold compresses and maintaining neutral wrist positions also help reduce inflammation and pain.
About