Oral nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to lessen inflammation inside the wrist joint. This reduces pain and other symptoms of carpal tunnel syndrome. Drugs like naproxen and ibuprofen can be used for up to a few weeks until symptoms subside. If they don’t help, other nonsurgical remedies are required.
Does Medicare Cover Carpal Tunnel Surgery?
From Dr. Z - Carpal tunnel syndrome specialist
Does Medicare Cover Carpal Tunnel Surgery?
Does Medicare cover carpal tunnel surgery? Yes it does! But Medicare will only pay for carpal tunnel release surgery that's medically necessary. And there are some out-of-pocket costs you will incur.
Medicare will pay for diagnostic tests and certain carpal tunnel treatments, including surgery. The out-of-pocket costs are associated with having diagnostic tests, treatments, and the actual surgery. But there are programs which can help you cover those added expenses.
In this article I will discuss what carpal tunnel syndrome is, the signs, and it's hallmark symptoms. I'll also show you how it’s diagnosed, and which nonsurgical and surgical treatment options are available.
Then I will outline how Medicare works, especially with the costs involved. You'll learn about additional programs that can help pay some or all of the extra costs involved.
You can also call Medicare using the telephone numbers listed at the end of this article.
Before we start, here are some insurance terms you need to know:
- Out-of-pocket is what you have to pay directly. This may or may not be reimbursed later.
- Deductible is the annual amount you must spend out-of-pocket before an insurer starts to pay anything.
- Coinsurance is the percentage of a treatment’s cost that you must pay out-of-pocket.
- Copayment is a set out-of-pocket amount you pay when receiving some treatments (usually prescription drugs).
Basics of carpal tunnel syndrome
Carpal tunnel syndrome is one of the most common disorders of the hand. It affects over 5 million Americans. It also accounts for 250,00 new cases each year.
This is why carpal tunnel surgery is the second most common elective surgery performed in the United States. But how does carpal tunnel syndrome happen? What are its symptoms? How is it diagnosed and treated? These are explained below.
How carpal tunnel syndrome happens
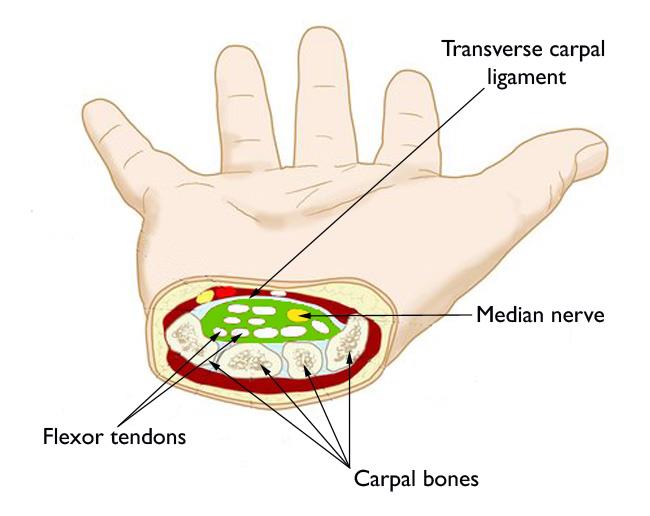
At its core, carpal tunnel syndrome is a neurological problem. The nerve involved is the median nerve. This nerve travels from the arm, through the wrist, and into the hand.
Inside the wrist, it passes through a narrow channel called the “carpal tunnel”. This channel is where the disorder gets its name.
But the median nerve is not alone in this passageway. It also has
flexor tendons running alongside it. These tendons are responsible for curling your fingers.
The carpal tunnel channel is already narrow and crowded enough. But sometimes, the tendons become irritated. And that leads to swelling.
Nobody is really sure why the tendons get irritated. But it’s likely due to performing repetitive tasks like typing, knitting or using tools makes the condition worse.
Whatever the cause of carpal tunnel syndrome, the result is that the tendons swell more and more. They swell and expand so much that they crush the adjacent median nerve.
It’s this nerve crushing that produces all of the abnormal symptoms of carpal tunnel syndrome.
Carpal tunnel symptoms
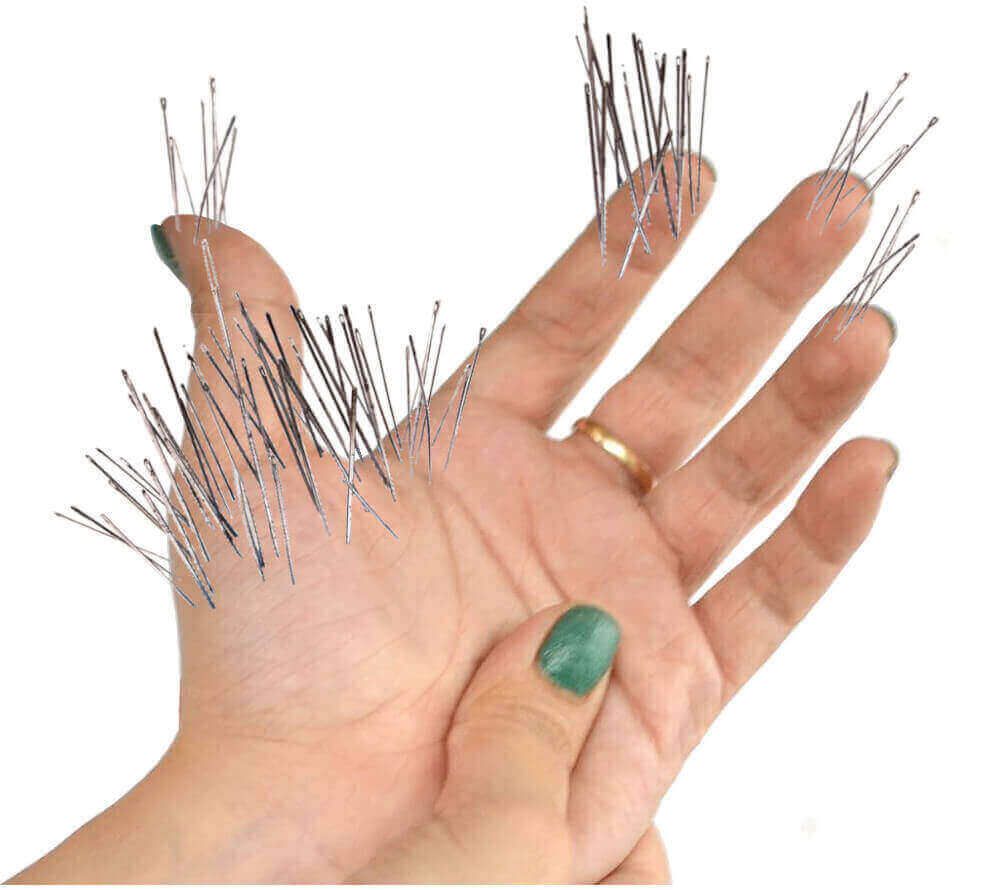
Carpal tunnel symptoms are always described as numbness, tingling (pins & needles), pain, weakness, soreness or burning. It occurs in the palm of the hand and all fingers except the little finger.
About 80% of the time, carpal tunnel syndrome affects both hands. This is called bilateral carpal tunnel syndrome.
When it starts out, symptoms are usually noticeable when the hand is resting. For instance, numbness, tingling or pain may wake you from a dead sleep to shake out your hand. But as the condition progresses, these symptoms persist into the daytime.
Symptoms can be persistent or intermittent. They can involve only one finger or all fingers and the palm. Sometimes they can radiate up the forearm. Other times pain can shoot like electric shocks.
Carpal tunnel symptoms can progress rapidly or slowly. Generally, it takes about 6 months for symptoms to advance from the mild stage, through the moderate stage, and into the severe stage. This is when symptoms are intense. You lose finger dexterity, hand strength, and the ability to feel hot or cold.
Diagnosing carpal tunnel syndrome
A carpal tunnel diagnosis begins by the doctor ruling out other candidate disorders that can cause hand problems. Tests for arthritis are first conducted. Then the doctor uses MRI or ultrasound to see if there’s an anomaly or abnormal structure inside your wrist joint.
Once other conditions are ruled out, doctors can diagnose carpal tunnel syndrome using a variety of tests. Chief among them are the “provocative tests”. These tests attempt to provoke or temporarily worsen symptoms you already have. If you feel symptoms worsening during the tests, then it’s positive for carpal tunnel syndrome.
These provocative tests are the Tinel, Phalen, and Durkan tests. You can actually perform these tests on yourself using these instructions.
Other methods doctors use to diagnose carpal tunnel syndrome are electrodiagnostic tests. These are nerve conduction studies of the median nerve and electromyography (EMG). Each test sends electrical impulses from the arm to the hand.
Primary nonsurgical treatments
Treating carpal tunnel syndrome is most successful when diagnosed early. Usually, when symptoms are mild, they can be completely eliminated with simple, nonsurgical treatments. These carpal tunnel treatments fall into the 5 categories below.
Oral drugs
Steroid shots
Night bracing
Stretching exercises
Myofascial release massage
Surgical treatments
All surgical treatments for carpal tunnel syndrome have one aim. That is, to cut the transverse carpal ligament. This ligament acts like a roof over the wrist bones. When it’s cut, the bones pull apart, allowing more room for the swollen tendons. This eases the crushing pressure on the median nerve.
There are two basic types of surgery for carpal tunnel syndrome. Both operative techniques use anesthesia that's either local (which numbs the hand) or general (which puts you to sleep). The surgery is usually performed on an outpatient basis in a hospital or surgical center.
The two techniques are called
open
and
endoscopic
carpal tunnel release surgery. Here's what they do and how they differ.
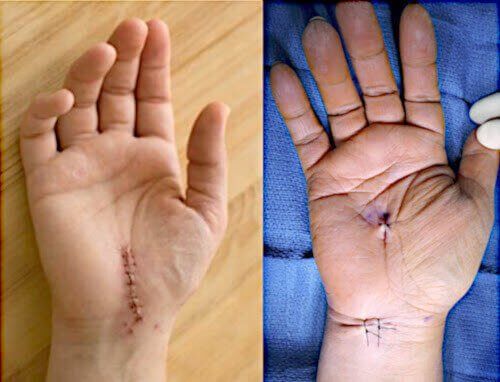
Open carpal tunnel release surgery
Endoscopic carpal tunnel release surgery
Recovery and prognosis
Complications of carpal tunnel surgery include excessive pain, bleeding, infection, and nerve injury. These can lead to partial loss of hand function.
Complete recovery from the open technique can take up to a year. Recovery from endoscopic surgery usually takes up to 2 months.
Approximately 50% of patients are satisfied with their surgical results by the third year. The other
50% are unsatisfied. They either have another corrective surgery (called “revision surgery”) or else find another
nonsurgical remedy to help.
Medicare coverage for carpal tunnel surgery
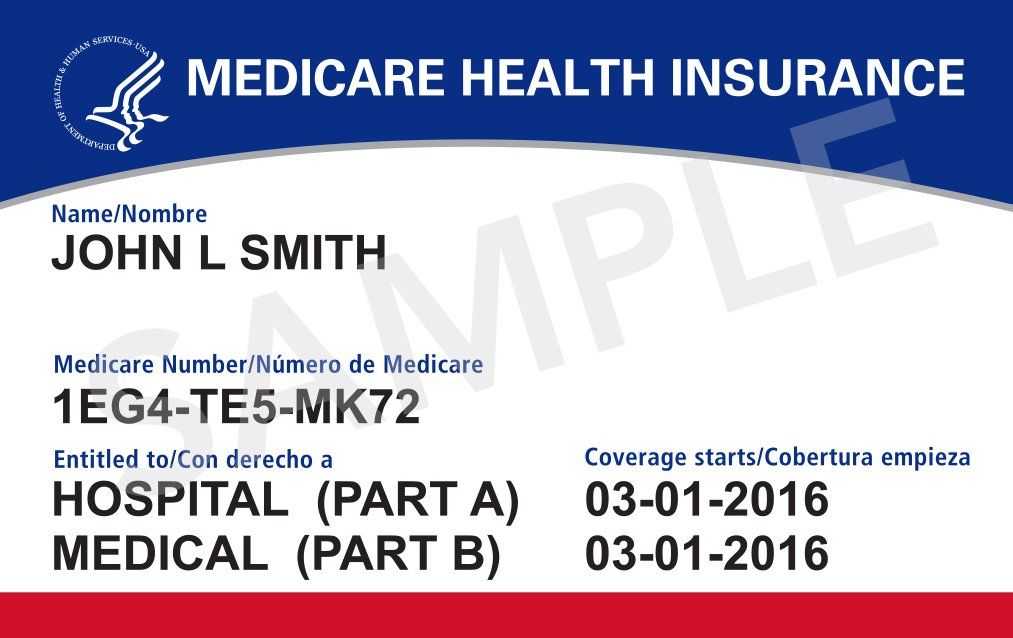
Medicare is actually a 4-part system of medical coverage. Each part (A, B, C, D) offers coverage in a specific area.
Part A and Part B of Medicare comprise what’s termed “Original Medicare”.
Part A is essentially hospital insurance. Part A covers carpal tunnel release surgery that involves a stay in the hospital.
Part B is essentially “other” medical insurance. Part B covers the following:
- All doctor visits
- All diagnostic tests
- Carpal tunnel surgery in an outpatient facility (hospital or surgical center)
- Certain nonsurgical treatments like steroid shots
Part C is also termed “Medicare Advantage”. It’s the alternative to Original Medicare. It offers the same basic benefits included in Part A and Part B. That means it includes covering costs for carpal tunnel surgery. Many Medicare Advantage plans also cover prescription drugs.
Part D is available for enrollment because Original Medicare doesn’t offer prescription drug coverage. When you enroll in a Part D plan, it will include most drugs required during and after carpal tunnel surgery.
A doctor may recommend using a prescription NSAID drug (like Meloxicam) before recommending surgery. If you have Original Medicare then you may receive prescription drug coverage if you enroll in a Part D plan. And if you have Medicare Advantage, then you may receive coverage with a plan that includes drug coverage.
Your out-of-pocket costs (what you pay)
Each Part of Medicare’s out-of-pocket costs change annually. Again, out-of-pocket means what you pay directly. The following are Medicare out-of-pocket costs for 2021:
Part A
When you have carpal tunnel surgery in a hospital, your Part A costs include:
- $1,484 deductible for each benefit period
- $0 coinsurance for days 1–60
Part B
If you require diagnostic tests (like EMG) or treatment for carpal tunnel syndrome in an outpatient facility, your Part B costs include:
- $148.50 monthly premium
- $203 annual deductible
- 20% coinsurance
Parts C & D
The costs for Parts C & D include copays, deductibles, coinsurance, and the monthly premiums. These costs can vary depending on your particular plan and the specific provider.
Programs that help with Medicare costs
There are programs to help Medicare patients pay their out-of-pocket costs. These programs are:
- Medigap: This is Medicare supplement insurance. It’s available to anyone enrolled in Original Medicare. Medigap pays 50–100% of Part A & Part B costs. There is a monthly premium which varies according to geographical location and individual circumstances.
- Extra Help: This program assists patients with paying Part D costs. It’s for people with limited income and resources. The program helps with approximately $5,000 per year to cover medicines.
- Medicaid: This is the well-known state & federal program to assist patients with low income and limited resources. It pays for some healthcare costs, but not all.
- Medicare Savings Programs:
These additional programs assist patients with limited income and limited resources. It’s designed to help pay premiums, coinsurance, and deductibles.
Before surgery, talk to your medical provider
Don't wait for surprises. Know exactly what your Medicare plan will cover and what won't. Unusually your doctor's office can help with that information. You can also contact Medicare directly at 1-800-633-4227.
If you have any other concerns if you need urgent information, call 1-800-MEDICARE (1-800-633-4227).
TTY/TTD users can call 1-877-486-2048.
The official Medicare portal is:
Conclusions
The two Medicare programs covering carpal tunnel surgery are Original Medicare and Medicare Advantage. They usually also pay for doctor visits, laboratory testing to confirm a diagnosis, and most nonsurgical therapies and treatments.