- Bend your wrist downward to a 90° angle, as far as you can.
- Firmly maintain the angle with your other hand.
- Hold for 30 seconds.
If symptoms appear or worsen, the test is positive for carpal tunnel.
CarpalRx - Carpal Pain Solutions
2609 S. Federal Highway
No. 1147 Fort Pierce, FL 34982
From Dr. Z - Carpal tunnel syndrome specialist
Table of Contents
Dr. M. Zannakis | The CarpalRx
Doctors test for carpal tunnel syndrome using two main methods: manual “provocative” exams you can do yourself (Phalen, Tinel, and Durkan tests), and electrodiagnostic exams like nerve conduction and EMG. Most patients start with self-tests and confirm results with a doctor.
Carpal tunnel syndrome is a neurological disorder caused by pressure on the median nerve inside your wrist. This nerve carries sensation and movement to your thumb, index, and middle fingers.
When surrounding flexor tendons become overworked or irritated, they swell and press on the nerve—leading to pain, tingling, and numbness. This is known as a repetitive stress injury.
Common triggers include:
The result is inflammation, swelling, and ultimately nerve compression—causing the hallmark symptoms of carpal tunnel syndrome.
Carpal tunnel often runs in families, suggesting a genetic component. But even without genetics, anyone who performs repetitive hand activities is at risk.
High-risk occupations and hobbies include:
While carpal tunnel syndrome isn’t technically curable,
it can be effectively managed. Most patients achieve lasting relief with consistent, nonsurgical therapy.
Before testing, be aware of these classic carpal tunnel symptoms:
Symptoms usually begin mildly—often waking you at night—and may progress to daytime pain and weakness. In advanced cases, patients lose sensitivity to heat and cold, The pain or numbness intensifies to the point of being described as "cruel" or "crushing". Weakness and loss of dexterity becomes progressively worse. When symptoms are constant and severe it's considered severe stage carpal tunnel syndrome. In 88% of cases, both hands are affected (bilateral carpal tunnel syndrome).
The first step is the manual provocative tests, which intentionally “provoke” your symptoms to confirm the diagnosis. These are the same tests doctors perform in their offices and can be done at home with a partner.
If one or more of these tests trigger numbness, tingling, or pain, it strongly suggests
carpal tunnel syndrome.

If symptoms appear or worsen, the test is positive for carpal tunnel.

If tapping causes tingling, numbness, or electric shock–like sensations, this indicates median nerve irritation from carpal tunnel.

If numbness or tingling appears, the test is positive.
If self-tests are positive, your doctor may confirm results with electrodiagnostic exams—specifically, nerve conduction and electromyography (EMG) tests.
These help evaluate the speed and strength of nerve signals traveling through your wrist.
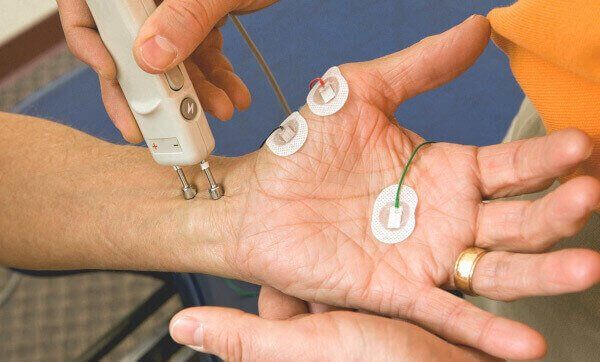
Electrodes are placed on your hand and wrist while small electrical impulses are sent through the skin.
A healthy median nerve sends signals quickly; a damaged one shows delayed responses.
Patients typically feel a mild static-like sensation during this painless test.

The EMG test uses fine needles inserted into thumb muscles to measure how well the nerve communicates with your muscles.
Although slightly uncomfortable, it lasts only a few minutes and provides detailed data about nerve health.
Note: Doctors often use electrodiagnostic tests to confirm, not replace, the results of manual exams. Provocative tests remain the most reliable indicators of carpal tunnel syndrome.
If your test results are positive, start therapy immediately. The American Academy of Orthopedic Surgeons recommends trying nonsurgical treatments first, since they are effective in up to 90% of patients.
In contrast, about half of all carpal tunnel surgery patients report incomplete relief or symptom recurrence within two years. The reasons for these poor results is either the patient did not respond to surgery, or they were misdiagnosed (which occurs in over 70% of cases).

Rest is your body's best healer. Limit activities that aggravate your wrists—like typing marathons, lifting heavy items, or repetitive hand motions.
If you can’t fully rest, take frequent one-minute breaks every hour and do gentle stretches during that time.

At night, we often bend our wrists unconsciously, which worsens nerve pressure.
Wearing a certified carpal tunnel night brace keeps your wrist neutral and allows healing.
Avoid generic pharmacy braces with a palmar spine—these can actually make symptoms worse.
And never wear a brace while working during the day; it restricts natural movement and can cause tendon strain.

They elongate tight tendons, reduce swelling, and restore circulation—relieving pressure on the median nerve.
Perform them several times a day, especially after repetitive hand use. Doctors recommend about one minute of stretching per work hour.

For moderate or severe symptoms, myofascial release massage is especially powerful.
Therapists use firm, rhythmic pressure to break down adhesions and drain excess fluid inside the wrist joint—both of which relieve pressure on the median nerve.
With daily therapy, even severe symptoms often resolve in 4–6 weeks.
Testing for carpal tunnel syndrome typically occurs in two phases:
If your tests are positive, don’t delay treatment. Early nonsurgical therapies—like rest, night bracing, stretching, and massage—can resolve most cases completely and prevent the need for surgery.
1. Can I test myself for carpal tunnel at home?
Yes. The Phalen, Tinel, and Durkan tests are simple self-checks that can reliably indicate carpal tunnel syndrome if they trigger numbness or tingling.
2. Are EMG and nerve conduction tests painful?
They may feel mildly uncomfortable but are not painful. These tests help confirm the diagnosis by measuring nerve signal speed and strength.
3. Can carpal tunnel heal without surgery?
In most cases, yes. With consistent nonsurgical care—such as night bracing, rest, and stretching—up to 90% of patients recover fully without an operation.

Dr. Maik Zannakis (Dr. Z)
Medical Director at the CarpalRx
Dr. Z is an acclaimed medical scientist renowned for his expertise in carpal tunnel syndrome and soft tissue disorders. With over 40 years of experience, he is credited with hundreds of medical journal publications and hundreds more web articles about carpal tunnel syndrome. After inventing the CarpalRx, Dr. Z became the go-to expert for carpal tunnel syndrome and wrist tendonitis. His opinions, inventions, and personalized care have distinguished Dr. Z as a trusted leader in this growing field. Read full Bio
Click here to learn more about Dr. Z
Email: dr.z@carplarx.com
Phone: 800-450-6118
CarpalRx - Carpal Pain Solutions
2609 S. Federal Highway
©2025 Copyright | All Rights Reserved | CarpalRX